Therapies
Common psychotherapies for bipolar disorder include cognitive behavioural therapy (CBT), family therapy, educational therapies, group therapy, and mindfulness. Click on the links or the tabs below to access the information, or browse via the drop-down menu on the left.
Image: ©Pixelrohkost – stock.adobe.com
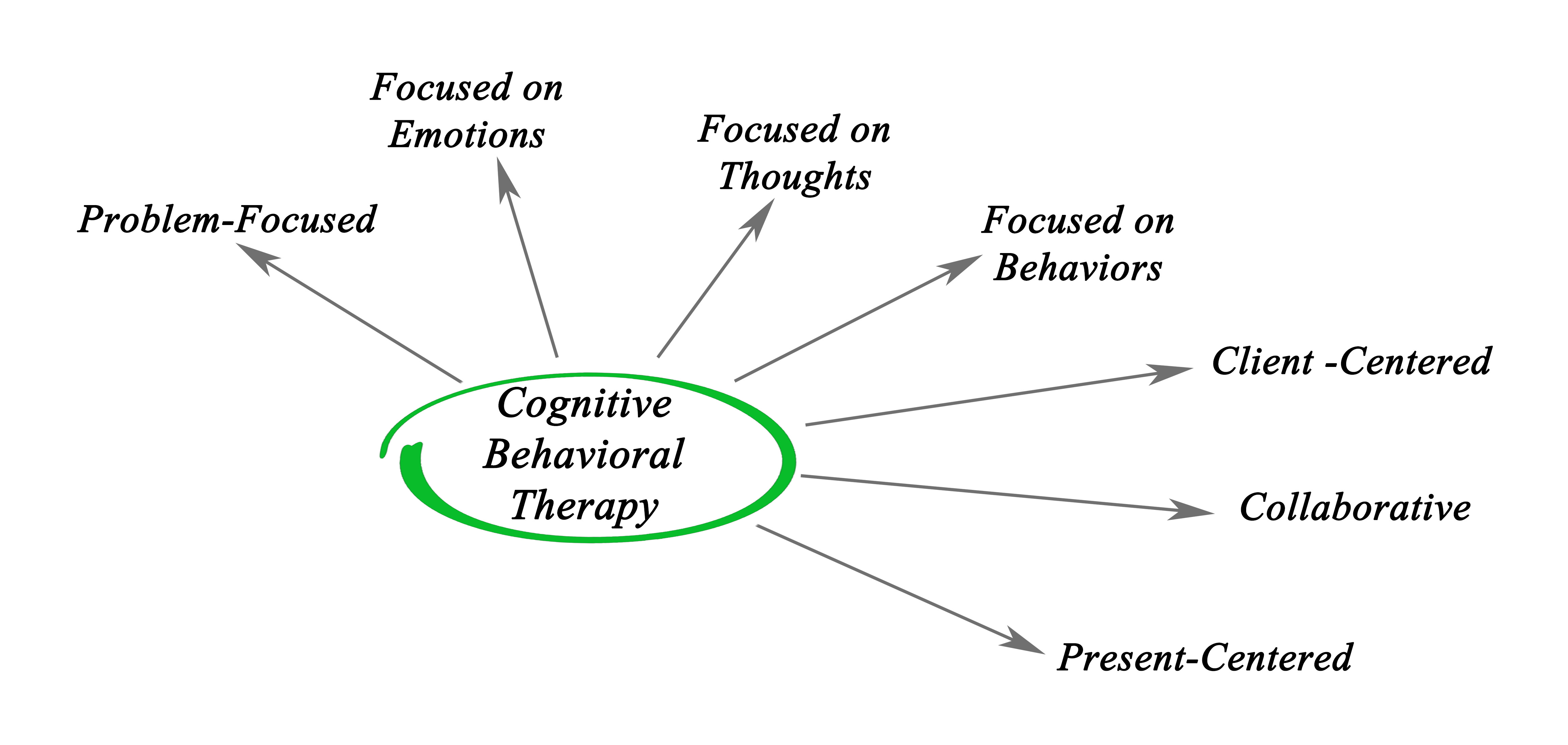
Cognitive behavioural therapy
What is cognitive behavioural therapy (CBT)? Psychosocial therapies such as CBT can provide a clinical adjunct to pharmacological therapy. CBT aims to generate links between patterns of thoughts, feelings and behaviours using cognitive restructuring to facilitate the understanding and management of these patterns. A variety of interventions can be labelled as CBT, but the primary approaches focus on coping strategies and problem solving skills. What is the evidence for CBT for bipolar disorder? Moderate quality evidence suggests CBT accompanied by medication for bipolar disorder can improve depression symptoms and functioning. Moderate to low quality evidence finds CBT can also improve…

Cost of therapies
What are the costs involved in treating bipolar disorder? Bipolar disorder is one of the leading causes of disability due to having a mental illness. A range of pharmacological and psychological interventions are effective in the management and prevention of acute episodes of bipolar disorder. However, these incur considerable costs, as well as productivity losses due to time off work. This topic presents the economic cost-effectiveness of psychosocial treatments in Purchasing Power Parity – International dollar (PPP-INT$), which is comparable to what the US dollar would buy in the United States. What is the evidence for psychosocial treatment costs? Moderate…

Crisis planning
What is crisis planning? People with severe mental illnesses such as bipolar disorder may be in need of emergency care at some stage in their illness. Crisis planning interventions focus on patients being involved in identifying preferences and planning for their future care during a mental health crisis. Crisis planning can help to prevent relapse by promoting better self-management and by prompting help-seeking. What is the evidence for crisis planning interventions? Moderate to high quality evidence suggests a small effect of reduced compulsory hospitalisation but not voluntary hospitalisation, for patients receiving crisis planning interventions for 12-24 months compared to standard…
Educational therapies
What are educational therapies? Educational therapies for psychiatric illnesses (psychoeducation) are targeted towards increasing a person’s knowledge about their disorder. Educational therapies aim to improve insight and understanding, promote coping and reduce stigma, increase medication adherence, enable behavioural change, and ultimately prevent relapse. Educational sessions can take place individually or in groups, with other patients or with family, and are usually incorporated into an ongoing treatment regimen in both hospital and community settings. What is the evidence for educational therapies? Moderate to low quality evidence suggests a medium-sized effect of fewer relapses to mania or depression with group psychoeducation, but…

Family intervention
What is family intervention? Family intervention involves the introduction of a patient’s immediate family into a psychosocial treatment setting. Its goals involve preventing relapse, improving the family’s relationships and understanding of the disorder as well as improving their own mental health, should that be compromised. Family interventions have a focus on psychoeducation which provides information on the disorder, medication, and treatment adherence. They can also employ cognitive and behavioural strategies to improve problem solving, communication skills, and coping, and to reduce high expressed emotion in the family unit. What is the evidence for family intervention? Moderate quality evidence finds family…

Group therapy
What is group therapy? Group therapy refers to any psychosocial therapy that is administered in a group setting. It can include specific cognitive or behavioural therapies and is often utilised in inpatient settings. The usefulness of group therapy has been examined in the context of improving illness outcomes such as symptom severity and quality of life, medication compliance, and particularly social interaction and anxiety. What is the evidence for group therapy? Moderate to low quality evidence finds medium to large effects of fewer relapses and improved symptoms and functioning following group therapies. Group therapies consisted of psychoeducation, cognitive behavioural therapy,…
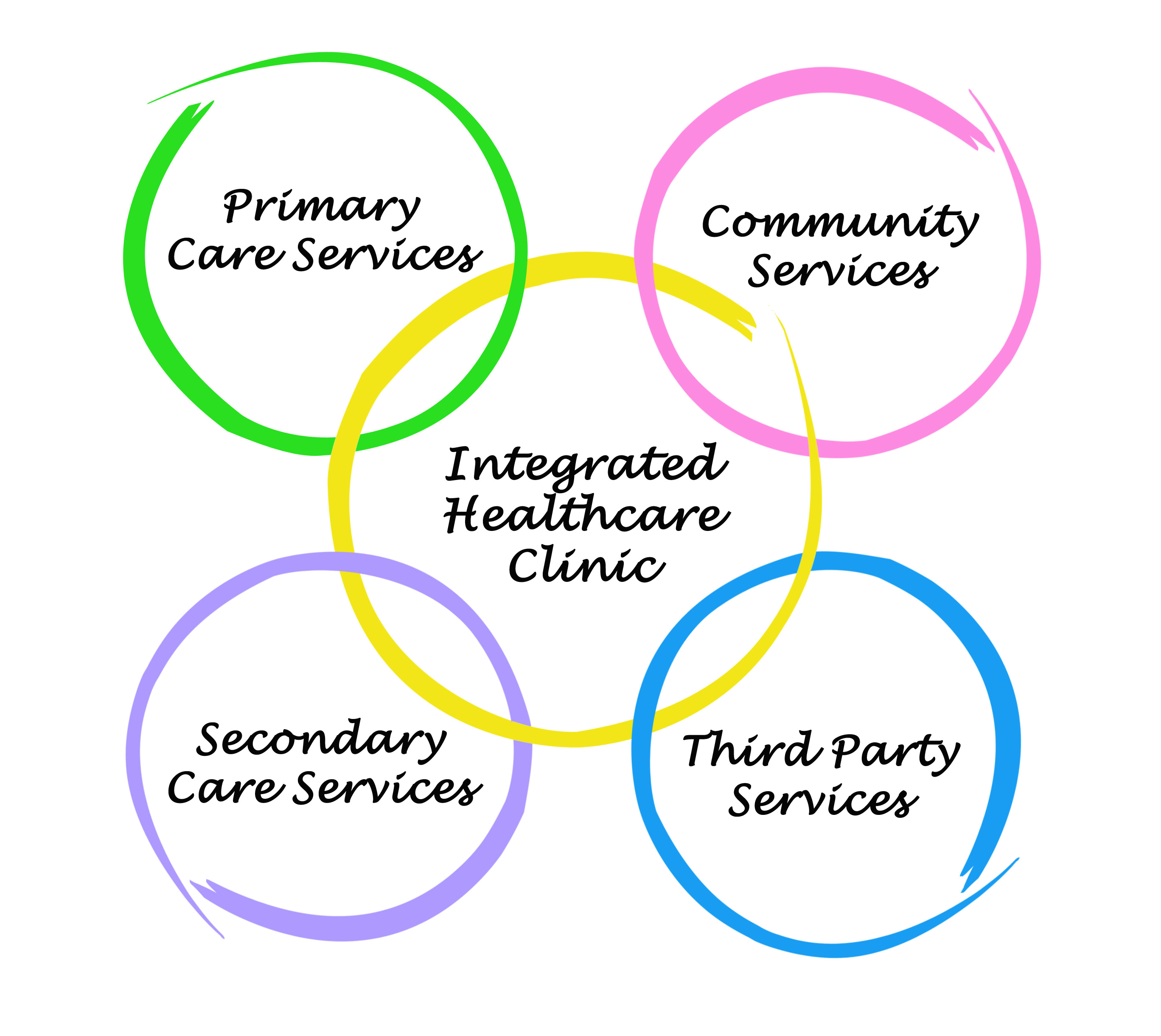
Integrated care
What is integrated care? Integrated care refers to the association of multiple treatment paradigms to produce a single unified program. The idea is to deliver seamless care to the patient to ensure high treatment continuity and improve patient satisfaction. Integrated programs typically involve multi-element psychosocial therapies for mental illness. For example, integrated psychological therapy may involve a combination of cognitive training, social skills training, problem-solving training and cognitive remediation. Integrated care can also refer to the formal liaison of typically distinct services such as medical practitioners and dedicated mental health teams, or the incorporation of mental health and substance use…

Interpersonal and social rhythm therapy
What is interpersonal and social rhythm therapy for bipolar disorder? The social environment can exert influence on synchronisation of circadian rhythms by entraining neurohormonal events such as cortisol and melatonin secretion. These are key components of circadian physiology, and disruptions to them can influence mood. Interpersonal and social rhythm therapy aims to improve interpersonal problem solving and social rhythm regularization. It involves psychoeducation about regulating routines and discussion around strategies for solving current interpersonal problems and preventing them in the future. What is the evidence for social rhythms interventions? Moderate to high quality evidence finds improved occupational, social, and general…

Mindfulness
What is mindfulness? Mindfulness involves intentional and non-judgmental focus of one’s attention on emotions, thoughts and sensations that are occurring in the present moment. The aim is to open awareness to present experiences, whether positive or negative, allowing thoughts to come and go without reacting, and accepting oneself and the experience. What is the evidence for mindfulness? Moderate quality evidence finds medium-sized improvements in depression and anxiety, but no consistent improvements in mania symptoms with mindfulness-based interventions in pre-post treatment assessments. There may also be improvements in mindfulness ability, stress, and emotion regulation following treatment. However, moderate to low quality…

Peer support
We have not found any systematic reviews on this topic that meet the Library’s inclusion criteria. Pending enough primary studies, we invite reviews on this topic to be conducted. Alternatively, we will endeavour to conduct our own review to fill this gap in the Library. November 2021 Image: ©yurolaitsalbert – Fotolia – stock.adobe.com

Shared decision making
What is shared decision making? Shared decision making aims to support people during specialist mental health treatment, encouraging them to be active in the decision making process regarding their pharmacological and psychoeducational treatment options, by keeping them informed and involved. Shared decision making interventions often utilise a decision-making tool, involving the person in the decision making process in conjunction with nursing support, ensuring that they understand the clinical problem, exploring their worries, fears, and expectations, discussing potential treatment options, and ensuring the implications of these options are understood. There is also provision for opportunities to review decisions. What is the…

Telemental health
What is telemental health? There is a growing need to deliver low-cost treatments tailored to individual needs and delivered in a continuous way (e.g. all year long) from any location. Telemental health has the potential to meet this need. Telemental health refers to any mental health treatment that is provided electronically, either by telephone or internet such as via online health programs, or video conferencing. This type of intervention involves structured counselling and generally aims to increase medication adherence and prevent relapse. Importantly, it also removes geographic barriers to care. What is the evidence for telemental health? Moderate to low…

Therapeutic relationships
What are therapeutic relationships in bipolar disorder? The therapeutic relationship refers to the relationship between a patient and a clinician. Many patients consider it to be the most important component of care, and therefore it should influence how well patients engage with services, and how well they show improvements from therapy. What is the evidence on therapeutic relationships? Moderate quality evidence suggests good therapeutic relationships can be associated with increased medication adherence and improved symptoms. November 2021 Image: ©ASDF – stock.adobe.com

User-held records
We have not found any systematic reviews on this topic that meet the Library’s inclusion criteria. Pending enough primary studies, we invite reviews on this topic to be conducted. Alternatively, we will endeavour to conduct our own review to fill this gap in the Library. June 2020

Vocational therapies
We have not found any systematic reviews on this topic that meet the Library’s inclusion criteria. Pending enough primary studies, we invite reviews on this topic to be conducted. Alternatively, we will endeavour to conduct our own review to fill this gap in the Library. June 2020
Green - Topic summary is available.
Orange - Topic summary is being compiled.
Red - Topic summary has no current systematic review available.
