Physical disorders
People with PTSD may also have co-occurring “comorbid” physical disorders. Common comorbid conditions include traumatic brain injury, chronic pain, and metabolic syndrome. Click on the tabs below to access all the information, or browse via the drop-down menu on the left.
Image: ©Kurhan – stock.adobe.com

Cancer
What is cancer and PTSD? Cancer is a broad group of diseases involving abnormal cell growth such that cells divide and grow forming malignant tumours. These may spread through the lymphatic system or blood stream. Not all tumours are malignant – some remain benign and do not invade other organs. Lifestyle, genetic factors and environmental pollutants increase a persons’ risk of developing cancer. Cancer can affect people of all ages. The most common cancers include lung cancer (22% of all cancers), bowel cancer (12%), breast cancer (8-23%) and prostate cancer (7%). Cancer may be measured by incidence or mortality rates….
Chronic fatigue syndrome
What is chronic fatigue syndrome and PTSD? Chronic fatigue syndrome is a widely accepted medical condition characterised by extreme fatigue. The fatigue lasts for at least six months, worsens with physical or mental activity, and does not improve with rest. The fatigue cannot be explained by an underlying medical condition. The causes of chronic fatigue syndrome are still being investigated, but may include viral infection and/or exposure to psychological stress. What is the evidence for chronic fatigue syndrome in people with PTSD? Moderate to low quality evidence finds a medium-sized effect of increased rates of chronic fatigue syndrome in people…

Chronic pain and fibromyalgia
What is chronic pain, fibromyalgia and PTSD? Pain is common in trauma patients, with greater frequency and severity of pain found when compared to people without PTSD. Fibromyalgia is also commonly reported, which is a centralised pain syndrome characterised by the presence of chronic widespread pain in association with fatigue, sleep disturbances, and cognitive dysfunction. What is the evidence for chronic pain in people with PTSD? Moderate to high quality evidence finds a small association between increased PTSD symptoms and increased chronic widespread pain. Lower quality evidence found a bidirectional associations between pain and PTSD symptoms within six months post-trauma….
Dementia
What is dementia and PTSD? Dementia is characterised by significant cognitive impairment. Symptoms include memory, executive functioning, language, and movement impairments, and an inability to identify objects, people, sound or smell. Other symptoms may include behavioural disturbances, anxiety, apathy, delirium, and mood and sleep disturbances. Mental disorders are associated with a high prevalence of psychiatric comorbidities, and aging may increase the risk of developing comorbidities such as dementia. What is the evidence for dementia? Moderate to low quality evidence finds a small increased risk of dementia in older veterans with PTSD compared to older veterans without the disorder. August 2021…

Diabetes
What is diabetes and PTSD? Diabetes is a state of impaired insulin function, either as a result of reduced insulin production (type 1 diabetes) or reduced insulin responsiveness (type 2 diabetes). Insulin regulates blood glucose levels, and reduced insulin function effectively increases blood glucose levels (hyperglycaemia). This is a dangerous state in the long term, and can ultimately damage the retina, kidneys, nerves, and blood vessels. It is also an established risk factor for cardiovascular diseases including coronary heart disease, major stroke subtypes, and deaths attributable to other vascular causes. Therefore, diabetes is an important comorbidity in people with mental…
Heart disease
What is heart disease and PTSD? People with mental disorders often show increased rates of co-occurring physical conditions such as heart disease. An increased risk of heart disease in people with PTSD may be a consequence of the disorder itself, as it is associated with dysfunction of the immunological system and excess inflammation. This in turn is associated with significant cardiovascular health problems. Unhealthy lifestyle factors such as smoking and poor diet may also contribute to any increased risk of heart disease. What is the evidence for heart disease? High quality evidence finds a small increased risk of coronary heart…
Irritable bowel syndrome
What is irritable bowel syndrome and PTSD? Irritable bowel syndrome is a common gastrointestinal disorder. It is characterised by chronic abdominal pain and a change in the frequency or form of stool. Its pathophysiology remains poorly understood but is thought to involve dysregulation of the hypothalamic–pituitary–adrenal axis, neuroendocrine alterations, and emotional hypersensitivity. Mechanisms that might underlie any association between post-traumatic stress syndrome and irritable bowel syndrome include hyperarousal, an exaggerated response to stress, and hypervigilance to bodily sensations. What is the evidence for irritable bowel syndrome? Moderate quality evidence finds a medium-sized effect of increased rates of irritable bowel syndrome…
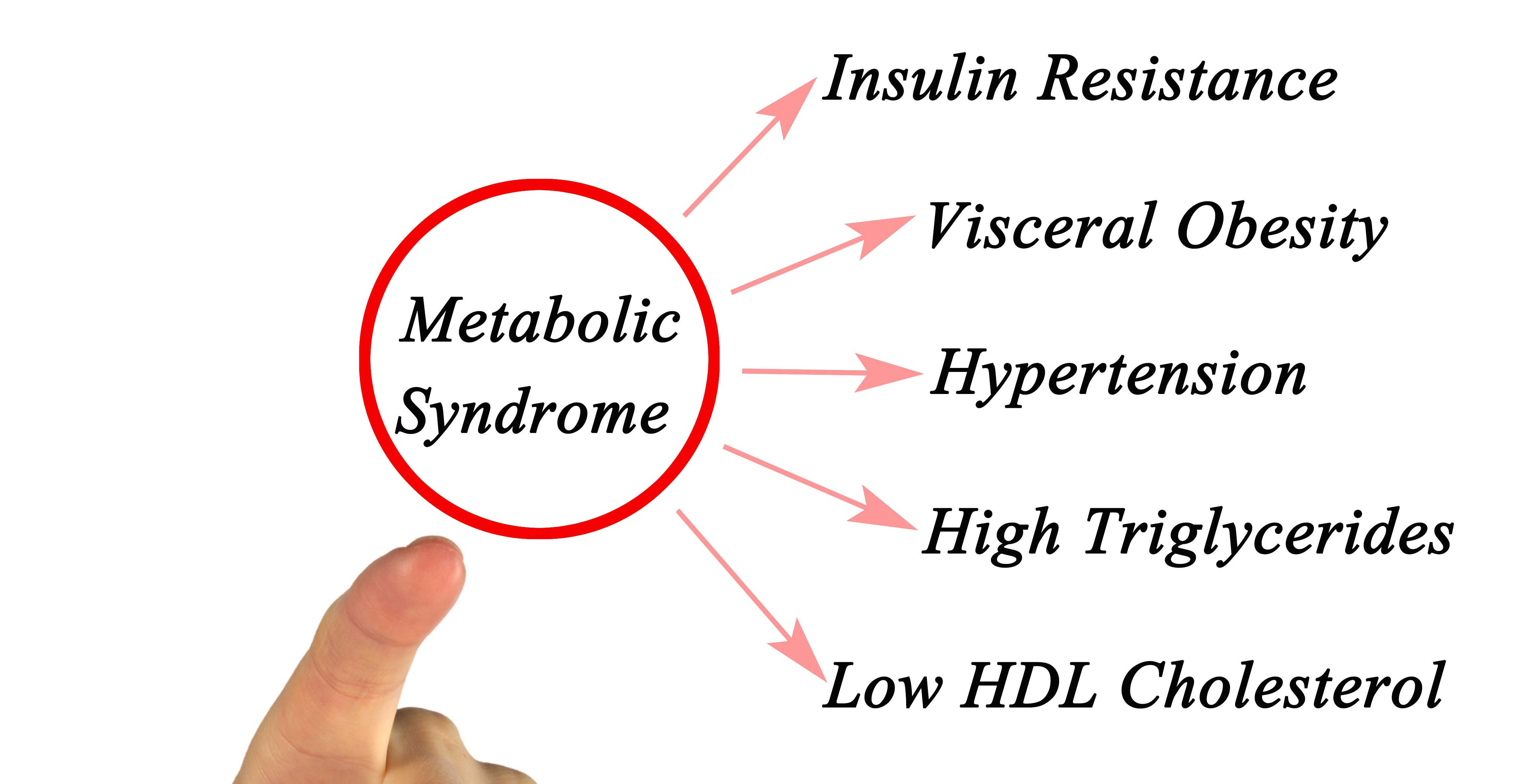
Metabolic syndrome
What is metabolic syndrome and PTSD? People with mental disorders often have increased rates of physical disorders, including metabolic syndrome. This syndrome is a risk factor for diabetes and cardiovascular diseases and is defined as a clustering of at least three abnormalities. These include obesity, high blood pressure, high blood triglycerides, low levels of high-density lipoprotein (HDL) cholesterol, and insulin resistance. Any increased risk of metabolic syndrome may be the result of unhealthy lifestyle factors, genetics, and factors associated with medications. What is the evidence for metabolic syndrome? High quality evidence finds a small to medium-sized increased risk of metabolic…

Obesity
What is obesity and PTSD? People with mental disorders often have increased rates of physical disorders, including obesity. This may be due to genetic factors, lifestyle choices, and metabolic effects of psychotropic medications. Obesity is defined as abnormal or excessive fat accumulation that presents a risk to health. A crude population measure of obesity is the body mass index (BMI), which is a person’s weight divided by the square of his or her height. A person with a BMI of 30 or more is generally considered obese. Being obese is a major risk factor for diabetes, cardiovascular diseases, and cancer….

Sleep apnea
What is sleep apnea and PTSD? People with mental disorders may show increased rates of co-occurring conditions such as sleep apnea. The most common form of sleep apnea is obstructive sleep apnea (OSA). OSA is seen in around 5-10% of the general population and occurs when the muscles of the upper airway relax in such a way that they block the airway during sleep. As a result, OSA is associated with daytime sleepiness, cognitive dysfunction, and the development of hypertension, cardiovascular disease, and abnormalities in glucose metabolism. OSA also has adverse effects on quality of life and can lead to…

Temporomandibular disorder
What is temporomandibular disorder and PTSD? The temporomandibular connects the jawbone to the skull. Disorders of the temporomandibular cause pain in the jaw joint and in the muscles that control jaw movement. Causes of temporomandibular disorder is often difficult to determine, but in most cases, the pain and discomfort is temporary and can be relieved with self-managed care or nonsurgical treatments. What is the evidence for temporomandibular disorder? Moderate to low quality evidence finds a medium-sized effect of increased rates of temporomandibular disorder in people with previous exposure to trauma, with or without PTSD. August 2021 Image: ©eddows – stock.adobe.com

Traumatic brain injury
What is traumatic brain injury and PTSD? Traumatic brain injury (TBI) is an alteration in brain function, or other brain pathology, caused by an external force. Brain injury can have severe consequences on physical, cognitive, and affective functioning and may lead to long-lasting limitations. Both civilian and military patients with TBI can develop PTSD, even when a person cannot recall the details of the traumatic event. What is the evidence for traumatic brain injury and PTSD? Moderate quality evidence found the prevalence of PTSD after a TBI was around 24%. Rates were higher in males than females, in samples with…
Green - Topic summary is available.
Orange - Topic summary is being compiled.
Red - Topic summary has no current systematic review available.
