Illness course and outcomes
The course and outcomes of schizophrenia vary widely between individuals. This category considers a range of outcomes in chronic, early and late-onset schizophrenia, and first-episode psychosis. Outcomes affecting day to day life include quality of life, relationships, culture, employment, homelessness, violence and self-harm, substance use, and recovery and relapse. Click on the tabs below to access all the information, or browse via the drop-down menu on the left.
Image: ©Pavel Timofeev – stock.adobe.com

Absconding
What is absconding in people with schizophrenia? Absconding refers to the departure of patients from hospital wards without permission. The definition of absconding can vary depending on the length of time required for an absence to be considered absconding, and on the method of departure (e.g. leaving a locked ward, leaving the hospital grounds, or failing to return from day leave). Absconding status is influenced by the patient’s admission, whether it be voluntary, involuntary, or legally detained. There are significant implications of absconding for patients, carers and family members. What is the evidence for absconding? Moderate to low quality evidence…

Age at onset
How is age at onset important to people with schizophrenia? Differences are observed in the age at onset of psychotic symptoms, which may be influenced by genetic or environmental risk factors, or sex. Understanding the factors that impact on age at the onset of symptoms could lead to better understanding of the risk factors for the disorder and earlier and improved intervention strategies. What is the evidence for age at onset of schizophrenia? Moderate to high quality evidence suggests the median age at onset of schizophrenia is around 25 years old. The incidence (i.e., new cases) of schizophrenia is higher…

Childhood and early-onset schizophrenia
What is childhood and early-onset schizophrenia? Childhood-onset schizophrenia has an onset prior to the age of 13 years, and early-onset schizophrenia has an onset between the ages of 13 and 17 years. What is the evidence on childhood and early-onset schizophrenia? Moderate quality evidence suggests poorer long-term functioning in children and adolescents with early-onset schizophrenia compared to other psychiatric disorders. August 2020 Image: ©Brian Jackson – Fotolia – stock.adobe.com

Creativity
How is creativity related to schizophrenia? A link between creativity and psychiatric disorders has long been postulated. This hypothetical connection has been the subject of many theoretical approaches, although theory and research results in this field are scattered and disparate. What is the evidence for creativity in people with schizophrenia? Moderate to low quality evidence finds a small association of lower creativity scores in people with schizophrenia compared to controls without a mental illness. August 2020

Criminal offending, aggression and violence
How is criminal offending, aggression and violence related to schizophrenia? Criminal offending covers a wide range of behaviours from destructive acts, stealing, sexual assaults, to physical assaults causing injury or death. The majority of people with schizophrenia will never commit a crime, however the few who do may help perpetuate a negative public stereotype that schizophrenia is associated with violent behaviour. It is difficult to determine whether any criminal acts committed by people with schizophrenia are a consequence of the illness or are traits of the particular individual. This is confounded by the fact that people with schizophrenia may be…

Criminal victimisation
What is criminal victimisation? Criminal victimisation refers to a person being the victim of a violent crime (rape or sexual assault, robbery, aggravated or simple assault) or a property crime (burglary and theft). People with a severe mental illness may be at higher risk of criminal victimisation. This may be a result of possible cognitive impairment (e.g. poor reality testing, judgment, social skills, planning, and problem solving), and sometimes compromised social situations (e.g. poverty, unemployment, homelessness, and social isolation). What is the evidence for criminal victimisation? Moderate quality evidence found increased rates of criminal victimisation in people with schizophrenia compared…

Cultural differences
How are cultural differences related to course and outcome of schizophrenia? Cultural differences may influence the course and outcome of illness for people with schizophrenia. These may be the result of differences in understanding of mental illness, and different attitudes and treatment approaches towards these disorders. Some cultures may provide more accessible pathways to care than others, including ready access to treatment and family and social support that can assist the individual to better deal with symptoms and any associated distress. Negative cultural attitudes towards mental illness may exacerbate stigma and social isolation, and some cultures may focus more on…

Diet
How is diet related to schizophrenia? People with mental disorders may be at increased risk of nutritional deficiencies due to poor diet. Poor diet is a major and modifiable cause of comorbid conditions, including metabolic syndrome and obesity. During pregnancy, it also contributes to the risk of developmental problems in the foetus. What is the evidence regarding diet ? Moderate to low quality evidence finds poor dietary patterns in people with schizophrenia, including decreased fibre and fruit intake, and increased energy, sodium and saturated fat intake compared to people without a mental disorder. People with schizophrenia may have high LDL…

Drug and alcohol use
What is comorbid drug and alcohol use? Drug and alcohol misuse, abuse or dependence are concerns for people with schizophrenia due to the association with poor clinical and social outcomes, including high rates of suicide, HIV, homelessness, aggression and incarceration. Moreover, substance use places additional burden on patients, families, psychiatric services, and government resources due to high rates of treatment non-adherence and relapse. This topic covers outcomes for people with schizophrenia and comorbid substance use (termed ‘dual diagnosis’). Please also see the topic on rates of comorbid substance use, as well as substance use as a risk factor for schizophrenia. What…

Duration of untreated psychosis
What is the duration of untreated psychosis (DUP)? DUP is generally determined as the time from the onset of psychotic symptoms to the initiation of treatment or first clinical presentation, when a diagnosis of first-episode psychosis may be given. Longer DUP has been associated with poorer prognosis (see the DUP and outcomes topic). As such, understanding the effects of DUP is particularly important because it is potentially modifiable. What is the evidence for DUP? Moderate to high quality evidence indicates the presence of an obligatory dangerousness criterion for compulsory treatment of mental illness is associated with longer DUP. Moderate quality…

Duration of untreated psychosis and outcomes
What is duration of untreated psychosis (DUP)? DUP is generally determined as the time from the onset of psychotic symptoms to the initiation of treatment or first clinical presentation, when a diagnosis of first-episode psychosis may be given. Longer DUP has been associated with poorer prognosis and is thought to be a predictor of the likelihood and extent of recovery. As such, understanding the effects of DUP is particularly important because it is potentially modifiable. What is the evidence for DUP and outcomes? Moderate to high quality evidence indicates longer DUP, particularly over 9 months, is associated with more severe…

Electronic device use
How is electronic device use relevant to schizophrenia? There is growing interest in using telemental health to support the treatment of schizophrenia. Telemental health refers to any treatment that is delivered electronically, such as via mobile devices, online health programs or video conferencing. This topic assesses rates of electronic device use to ascertain whether telemental health treatments would be viable for people with schizophrenia. What is the evidence for electronic device use? Moderate quality evidence suggests around 66% of people with schizophrenia use mobile phones, with the rate increasing to 81% in the most recent studies. Attitudes are generally positive…

Employment
How is employment related to schizophrenia? Employment rates are typically low and can be used as a measure of social disability in schizophrenia. Employment function is commonly assessed using outcomes such as rates of employment, success in getting and keeping employment, as well as patient characteristics and the treatments received. Low rates of employment among people with schizophrenia places extended burden on social support and disability services, and significantly affects quality of life. Employment rates may be improved by greater focus on patient education and opportunities for supported employment. What is the evidence regarding employment? Reviews with moderate or moderate…

First-episode psychosis
What are outcomes for people with first-episode psychosis or high-risk mental states? After being identified as having high-risk mental states, or after an initial diagnosis of psychosis, relevant outcomes over the years following include transition to psychosis or schizophrenia, symptom severity, recovery and remission, relapse, employment, functioning, relationships, and quality of life. Investigating these outcomes and the factors influencing them provides insight into early treatment strategies. What is the evidence for outcomes in people with first-episode psychosis or high-risk mental states? Moderate quality evidence suggests up to 80% of people have good or intermediate outcomes following a first episode of…

Functional outcomes
What are functional outcomes? Functional outcomes include work performance, relationships, and living skills which may be adversely affected by schizophrenia. Developing coping skills to manage general life stressors and illness complications may help improve functional outcomes. What is the evidence for functional outcomes? Moderate to high quality evidence finds small associations between better functioning after treatment for first-episode psychosis and shorter duration of untreated psychosis, less severe symptoms (both at baseline and after treatment), better premorbid functioning, better cognitive functioning, more education, longer work history, and female gender. Moderate quality evidence finds more severe negative symptoms are associated with poorer…

Homelessness
How is homelessness related to schizophrenia? Many studies have reported a high prevalence of various health problems, including mental health problems, among homeless people. However, the rate of schizophrenia in this population may be difficult to measure due to diversity between studies in the definitions of homelessness and the diagnostic criteria used for schizophrenia. What is the evidence for homelessness? Moderate to high quality evidence found the prevalence of schizophrenia spectrum disorders was around 12.4% in high-income countries and 22% in developing countries. The prevalence rate of any psychotic disorder in homeless people was around 21%. Rates of schizophrenia were…

Hope
How is hope related to schizophrenia? Hope is a basic element of human existence, and is necessary for healthy coping. Hopelessness has been identified as a core characteristic of both depression and schizophrenia and may contribute to chronicity of the disorder. Once established, hopelessness may become a central limiting factor in the efficacy of treatment and rehabilitation of patients and can also adversely affect carers and significant others. What is the evidence relating to hopelessness? Moderate to low quality evidence suggests associations between increased hope and increased power, self-perception, insight, and quality of life. August 2020
Late-onset schizophrenia
What is late-onset schizophrenia? Late-onset schizophrenia is defined as onset of psychosis after age 45 years and it has been previously associated with a higher proportion of women, high levels of occupational functioning and marital relationships, as well as more severe paranoid delusions and more visual, tactile, and olfactory hallucinations. It has also been associated with less severe disorganisation and negative symptoms. What is the evidence relating to late-onset schizophrenia? Moderate quality evidence suggests negative life events, history of psychotic symptoms, poor social networks, cognitive impairment, and functional limitations are related to increased rates of late-onset schizophrenia. August 2020

Loneliness
How is loneliness related to schizophrenia? Loneliness is a subjective experience that arises when a person perceives their relationships to be inadequate to meet their need for belonging. It affects everyone from time to time, however people with psychotic disorders such as schizophrenia may be particularly vulnerable as they often report poor social networks and lower social support. What is the evidence on loneliness? Moderate to high quality evidence suggests increased positive symptoms, negative symptoms, depression, low perceived social support, internalised stigma, and low self-esteem are associated with increased feelings of loneliness. Moderate quality evidence suggests low quality of life,…

Mortality
How are mortality rates related to people with schizophrenia? The life expectancy of people with schizophrenia is reduced compared to the general population. The reasons for increased mortality in schizophrenia are largely unclear, but may in part be related to lifestyle factors such as weight gain, smoking, unhealthy diet and low physical activity levels. Schizophrenia may also be associated with increased risk of suicide. What is the evidence relating to mortality rates? Moderate to high quality evidence finds a medium-sized increased rate of mortality in people with schizophrenia compared to general population rates, with life expectancy being around 65 years…

Parenthood
What are the issues concerning parenthood for people with schizophrenia? People with schizophrenia have reduced fertility rates compared to general population rates. There is interest in determining how genetic factors predisposing people to schizophrenia are maintained in the face of these reduced fertility rates and this could be explained by increased fertility rates in unaffected relatives. Antipsychotic use in pregnant women requires careful consideration of the mother’s risk of illness relapse, against the risk of harm or complications for the developing infant (including congenital malformation, or poor obstetric outcomes) if medication is to be continued. However, there is currently very…
Pathways to care
What are pathways to care? The help-seeking efforts made by an individual and their families when symptoms of psychosis are apparent, and the clinical services made available as a result of these efforts, are collectively known as ‘pathways to care’. Pathways to care can also encompass service structures that have not been actively sought by the individual. Understanding pathways to care may improve early intervention strategies and contribute to reducing the duration of untreated psychosis. What is the evidence for pathways to care? Moderate to low quality evidence suggest young people have around three contracts before receiving specific services for…

Physical activity
How is physical activity relevant to people with schizophrenia? Individuals with a serious mental illness are more likely to be sedentary than the general population and are consequently at high risk for chronic medical conditions associated with inactivity. Physical activity has the potential to improve quality of life for people with schizophrenia. Positive psychological effects from physical activity in clinical populations have been reported, including improved quality of life. What is the evidence for physical activity in people with schizophrenia? Moderate to high quality evidence suggests people with a psychotic disorder, and those with at-risk mental states, were less active,…

Physical health monitoring
How is physical health monitoring relevant to people with schizophrenia? People with severe mental disorders can be at increased risk of a number of physical conditions. This may be due to lifestyle factors such as poor diet and lack of exercise, but also some treatments for schizophrenia can have adverse physical side effects. Furthermore, people with schizophrenia may be hesitant to seek medical advice. What is the evidence for physical health monitoring? Moderate quality evidence finds people with any severe mental disorder such as schizophrenia, bipolar disorder, or major depression, are prescribed medication for physical disorders less often than people…
Psychotic relapse
What is psychotic relapse? Psychotic relapse is the reoccurrence of previously treated psychotic symptoms. Effective early recognition may offer the potential for early intervention to prevent relapse, such as medication adjustment, psychosocial treatments, social support and stress reduction. Early warning signs are subjective experiences, thoughts and behaviours that occur immediately prior to a psychotic relapse, which signal to the patient or their family that their condition is deteriorating. It is important that these early signs be identifiable by family members or carers, as patients may minimise or disguise these symptoms in order to appear healthy or to avoid hospital readmission….

Quality of care
What is quality of care? Quality of care refers to the standards of treatment provided to people with schizophrenia. This topic considers not only the availability of various types of treatment, but also the factors influencing successful treatment outcomes in physical and mental health-care models. What is the evidence for quality of care? Moderate to low quality evidence finds essential structural indicators for ensuring high quality health care delivery include the assessment of psychiatric and somatic comorbidity, length of hospitalisations, employment outcomes, and information exchange. Essential quality indicators for patient-related assessment of treatment outcomes include the frequency of access to…
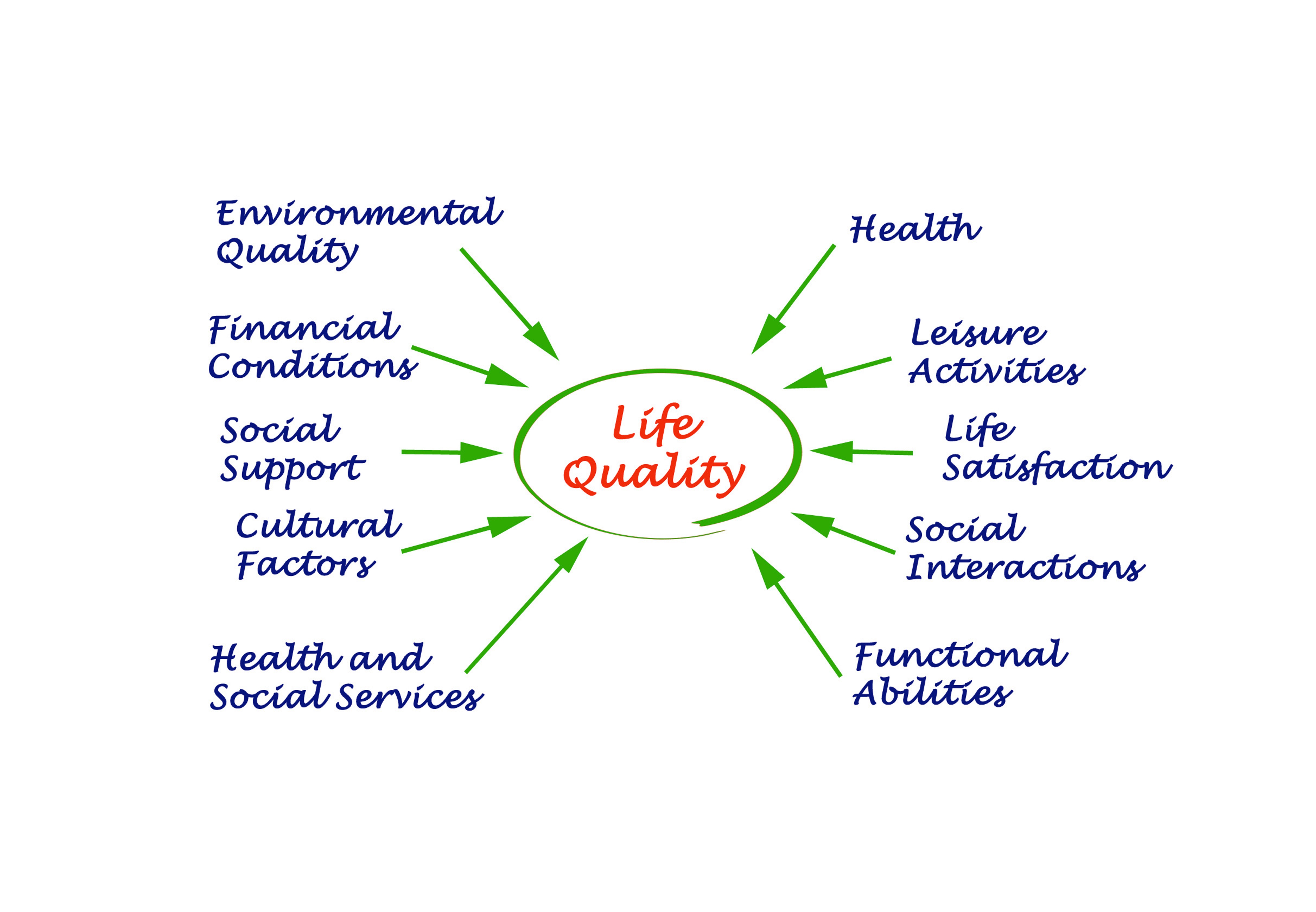
Quality of life
What is quality of life? Quality of life refers to an individual’s sense of satisfaction with their circumstances. This can be measured subjectively via interview and objectively via measures of overall health, social and material well-being and access to resources and opportunities. A key focus of quality of life research in schizophrenia is to identify factors that influence or predict a person’s satisfaction with their circumstances, which may then provide targets for therapeutic focus to improve quality of life. What is the evidence for quality of life? Moderate to high quality evidence finds large effects of poorer psychological, physical, and…

Relationships
How are relationships impacted by schizophrenia? Schizophrenia can have an intrusive effect on personal relationships, social interactions and on libido. For people with schizophrenia who experience difficulty forming and maintaining relationships, this may be a direct consequence of the disorder and its debilitating symptoms. Investigations have found that cognitive deficits experienced by many people with schizophrenia, including impairments in social perception and emotional recognition, may also pose hindrance to the formation of meaningful relationships. Antipsychotic medication has also been shown to impact on sexual function. What is the evidence on relationships? Moderate to high quality evidence finds a medium-sized association…

Religiosity
What is religiosity? Religiosity refers to religious activity, dedication, and beliefs. Religious themes are often reported in the content of delusions and hallucinations experienced by people with schizophrenia. What is the evidence for religiosity? Low quality evidence is unable to determine any consistent relationships between religion and delusions or hallucinations. August 2020

Remission and recovery
How are remission and recovery defined? Remission has been defined as a level of symptomology that does not interfere with an individual’s behaviour, and is also below that required for a diagnosis of schizophrenia. Symptom improvements should last for a minimum of six months in order for remission to be reached. Recovery is less precisely defined. In addition to the symptom improvements required for remission, improvements in social and functional dimensions are required. These domains usually include, but are not restricted to; functional independence, maintaining satisfying relationships, being productive, having a sense of empowerment, and overcoming feelings of internalised stigma….

Sex differences
We have not found any systematic reviews on this topic that meet the Schizophrenia Library’s inclusion criteria. Pending enough primary studies, we invite reviews on this topic to be conducted. Alternatively we will endeavour to conduct our own review to fill this gap in the Library.

Smoking
How is smoking related to schizophrenia?Tobacco smoking is very common among people with schizophrenia, who often have particularly heavy use. This poses considerable health risks, may interfere with antipsychotic medications, and may place a financial burden on the individual. Heavy cigarette use may contribute to the increased mortality and reduced life expectancy reported within the schizophrenia population. This topic considers the effects of smoking among people with schizophrenia. Please also see the smoking topic in comorbid conditions for the rates of smoking in this population. What is the evidence for smoking in people with schizophrenia? Moderate to high quality evidence…

Stigma and attitudes towards mental health
What is stigma? There are three interacting levels of stigma: social, structural, and internalised. Social (public) stigma occurs within a large group, such as members of the general public, who collectively adopt stereotypes about the victims of stigma. Structural stigma refers to the institutional rules, policies, and procedures that restrict the rights and opportunities of particular groups of people. Internalised stigma occurs within an individual, such that a person’s attitude may reinforce a negative self-perception of mental disorders, resulting in reduced sense of self-worth, anticipation of social rejection and often a desire for social distance. For many people with schizophrenia,…

Suicide and self-harm
How is suicide and self-harm related to schizophrenia? Rates of suicide and self-harm are considerably higher in people with schizophrenia compared to the general population. There has been much research dedicated to determining these rates and also the potential risk factors, which have important applications for prevention. Many of the risk factors for suicide in the general population apply to people with schizophrenia, including depression, or having a history of attempted suicide or self-harm. However, factors specific to schizophrenia may also contribute to an increased risk of suicide or self-harm. What is the evidence relating to suicide and self harm?…

Treatment adherence
What is treatment adherence? Treatment adherence involves taking prescribed treatments (both pharmaceutical and psychosocial) as recommended by the treating physician. What is the evidence for treatment adherence? Moderate to high quality evidence found around 56% of people with schizophrenia were non-adherent to medication at some point. Moderate quality evidence found the dropout rate from psychosocial treatments was around 13%. Moderate to low quality evidence finds no differences in the rates of refusal of treatment or premature termination of treatment between people offered antipsychotics alone and people offered antipsychotics plus psychotherapy. There were also no differences in adherence rates between people…

Treatment-resistance
What is treatment resistance? Antipsychotic medications generally provide symptom relief and improvement in quality of life for people with schizophrenia. However, some people with schizophrenia find that antipsychotic medications do not provide adequate relief from their symptoms. This topic covers the course and outcome of treatment resistance, please see the treatment topics for information on potential treatments for treatment-resistant schizophrenia. What is the evidence on treatment-resistant schizophrenia? Moderate quality evidence finds people with treatment-resistant schizophrenia have higher rates of smoking, alcohol or substance abuse, suicide ideation, more glutamatergic abnormalities, and more familial loading for schizophrenia than people with treatment-responsive schizophrenia….
Green - Topic summary is available.
Orange - Topic summary is being compiled.
Red - Topic summary has no current systematic review available.
