Physical disorders
People with schizophrenia may have co-occurring (comorbid) disorders. Common physical comorbid conditions include heart disease, metabolic syndrome, and visual impairment, but lower rates of some cancers. Click on the links or the tabs below to access the information, or browse via the drop-down menu on the left.
Image: ©Kurhan – stock.adobe.com

Auditory system dysfunction
How is auditory dysfunction relevant to schizophrenia? People with schizophrenia may show increased rates of unrelated co-occurring conditions. These may include dysfunction of the auditory system or structural abnormalities of the ear canal. What is the evidence for comorbid auditory dysfunction? Moderate to low quality evidence is unclear of the prevalence of auditory system dysfunction in people with schizophrenia. June 2020

Autoimmune diseases
What are autoimmune diseases? People with schizophrenia may show increased rates of co-occurring conditions. Autoimmune diseases are caused by an overactive immune system. Some of the more common autoimmune diseases include; Celiac disease where the immune system reacts to gluten found in wheat and other grains; lupus, which affects skin, muscles, joints, lungs, heart and kidneys; rheumatoid arthritis, where bone and cartilage are damaged; Graves’ disease, where the thyroid gland is overactive; multiple sclerosis, where the nervous system is affected; type 1 diabetes, where the pancreas does not produce enough insulin to manage blood sugar levels. What is the evidence…
Blood disorders
How are blood disorders relevant to schizophrenia? People with schizophrenia may show increased rates of co-occurring conditions. These can include disorders of the blood, such as leukocytosis (excess leukocytes), hypokalemia (reduced potassium), and neutropenia (low neutrophil levels). What is the evidence for comorbid blood disorders? Moderate quality evidence suggests the incidence of mild neutropenia in people taking the antipsychotic clozapine is around 3.8%, and the incidence of severe neutropenia is around 0.9%. Death from neutropenia is rare at around 0.013%. Moderate to low quality evidence is unclear as to the rates of other blood disorders in people with schizophrenia. June…

Cancer
How is cancer related to schizophrenia? Cancer is a broad group of diseases involving abnormal cell growth, where cells divide and grow forming malignant tumours. Cancer may spread through the lymphatic system or blood stream. Lifestyle, genetic factors and environmental pollutants increase a persons’ risk of developing cancer. People with schizophrenia show increased exposure to risk factors associated with cancer, such as smoking, physical inactivity, poor diet, obesity, substance abuse, diabetes and hepatitis. What is the evidence for comorbid cancer? Moderate to high quality evidence finds a small increase in the rate of breast cancer in females with schizophrenia compared…
Cerebrovascular disease
How is cerebrovascular disease related to schizophrenia? People with schizophrenia may show increased rates of co-occurring conditions when compared to general population rates. Cerebrovascular disease includes strokes, transient ischemic attacks, aneurysms, and vascular malformations. A stroke happens when blood flow to the brain is interrupted due to a blocked artery (ischaemic stroke) or when an artery bursts (haemorrhagic stroke). A transient ischemic attack is similar to a stroke, but less severe, and an aneurysm involves an enlarged artery caused by weakness in the arterial wall. These can all cause brain damage if cells do not get enough of the oxygen…
Dementia
What is dementia? Symptoms of dementia include memory, language and movement impairment. People with dementia may also be unable to identify objects, people, sound or smell. There is often impaired executive functioning, for example, an inability to think abstractly, plan, initiate or stop actions. Other symptoms include behavioural disturbances, anxiety, apathy, delirium, and mood and sleep disturbances. Schizophrenia is also often associated with cognitive and functional decline; however, people with dementia show greater cognitive impairment. What is the evidence for comorbid dementia? Moderate quality evidence finds a medium-sized increased risk of dementia in people with schizophrenia. Studies conducted in non-European…

Dental disease
How is dental disease related to schizophrenia? Oral health is an important part of overall physical health. People with severe mental illness are susceptible to oral disease for a number of reasons which may include poor oral hygiene, concern about dental costs, difficulty in accessing healthcare facilities, and the side-effects of psychiatric drugs such as dry mouth. What is the evidence for comorbid dental disease? Moderate quality evidence suggests people with schizophrenia have more decayed and missing teeth and fewer filled teeth than people without schizophrenia. June 2020

Diabetes
How is diabetes related to schizophrenia? People with schizophrenia may show increased rates of unrelated co-occurring illnesses, one example is diabetes. Diabetes is a state of impaired insulin function, either as a result of reduced insulin production (type I diabetes) or reduced insulin responsiveness (type II diabetes). Insulin regulates blood glucose levels, and reduced insulin function effectively increases blood glucose levels (hyperglycaemia). This is a dangerous state in the long term, and can ultimately damage the retina, kidneys, nerves and blood vessels. Consequently, effective management of diabetes is crucial. It is unclear if any increased risk in people with schizophrenia…

Digestive disorders
How are digestive disorders related to schizophrenia? People with schizophrenia may show increased rates of co-occurring conditions, including appendicitis, gastric ulcers, irritable bowel syndrome, or celiac disease. What is the evidence for comorbid digestive disorders? Moderate to high quality evidence finds small increases in rates of anemia and celiac disease in people with schizophrenia or other psychotic disorders compared to people without a psychotic disorder. There were also increased rates of schizophenia in people with celiac disease compared to people without celiac disease. There were no increases in rates of Crohn’s disease or ulcerative colitis. Moderate to low quality evidence…
Epilepsy
What is epilepsy? People with schizophrenia may show increased rates of co-occurring conditions. These include epilepsy, which is a neurological disorder characterised by recurrent seizures. There are several types of seizures; focal or partial seizures are subtle and may go unnoticed as mild activity starts in one area of the brain and can spread to other areas. Generalised seizures are more severe, involve both hemispheres simultaneously and result in loss of consciousness. There are also ‘epileptic spasms’ that are of unknown origin. What is the evidence for epilepsy? Moderate quality evidence suggests the prevalence rate of schizophrenia or interictal psychosis…
Heart disease
How is heart disease related to schizophrenia? People with schizophrenia may show increased rates of co-occurring conditions, including heart disease. It is unclear if any increased risk is a consequence of the metabolic impact of antipsychotic administration or unhealthy lifestyle choices, or most likely, a combination of both. What is the evidence for comorbid heart disease? Moderate quality evidence finds small increases in rates of coronary heart disease and congestive heart failure in people with schizophrenia, with rates gained from both longitudinal and cross-sectional studies, and from data adjusted for potential confounding factors. Longitudinal studies with adjusted data also show…
Infectious diseases
How are infectious diseases related to schizophrenia? Infectious diseases include the human immunodeficiency virus infection (HIV), and hepatitis viruses, such as hepatitis B and hepatitis C. Schizophrenia is associated with an increased risk of these infectious diseases when compared to the general population. What is the evidence on infectious diseases in people with schizophrenia? Moderate to low quality evidence finds medium-sized increased rates of hepatitis B and C in people with schizophrenia compared to people without schizophrenia. Moderate quality evidence finds the prevalence rate of HIV in people with any severe mental illness, including schizophrenia, is around 8%. For hepatitis…
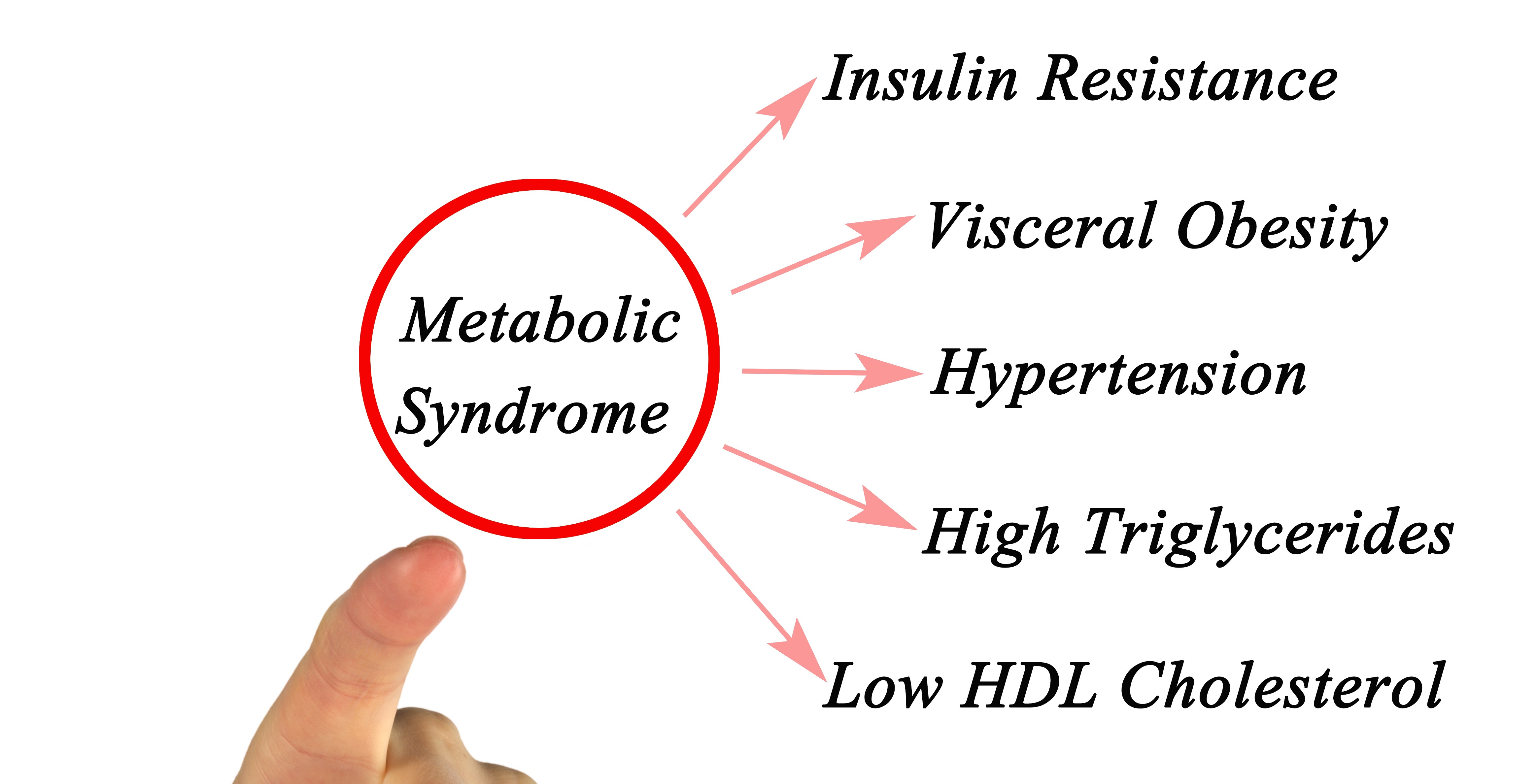
Metabolic syndrome
How is metabolic syndrome related to schizophrenia? Metabolic syndrome is a risk factor for diabetes and cardiovascular diseases. It is defined as a clustering of at least three abnormalities including obesity, high blood pressure, high blood triglycerides, low levels of high-density lipoprotein (HDL) cholesterol and insulin resistance. What is the evidence for metabolic syndrome in people with schizophrenia? Moderate quality evidence finds an overall prevalence of metabolic syndrome of around 32% in people with schizophrenia. Compared to age and gender-matched population controls, there are increased rates of abdominal obesity, hypertension, hypertriglyceridemia, and low HDL cholesterol, and no differences when compared…

Musculoskeletal and connective tissues
How are musculoskeletal and connective tissue abnormalities related to schizophrenia? People with schizophrenia show increased rates of co-occurring conditions, including various disorders affecting the musculoskeletal system. Common disorders include; osteoporosis and the less severe osteopenia, which occur when bones lose minerals more quickly than the body can replace them, causing a loss of bone thickness; rheumatoid arthritis and systemic lupus erythematosus result from a malfunctioning immune system that mistakenly attacks healthy tissue; and ankylosing spondylitis is a type of inflammatory arthritis that mainly affects the spine. What is the evidence for comorbid musculoskeletal and connective tissue abnormalities? Moderate quality evidence…

Obesity
How is obesity related to schizophrenia? People with a severe mental illness are at increased risk of obesity, which may be due to genetic and/or socio-economic factors, lifestyle choices, or metabolic effects of psychotropic medications. Obesity is defined as abnormal or excessive fat accumulation that presents a risk to health. A crude measure of obesity is the body mass index (BMI), which is a person’s weight divided by the square of his or her height. A person with a BMI of 30 or more on metric measures is generally considered obese. Being obese is a major risk factor for diabetes,…
Optical alterations
How are optical alterations related to schizophrenia? People with schizophrenia may show increased rates of co-occurring conditions. These can include short-sightedness (impaired long distance sight) and long-sightedness (impaired near distance sight), as well as reductions in the peripapillary retinal nerve fibre layer, and in macular thickness and volume. What is the evidence for optical alterations in people with schizophrenia? Moderate quality evidence finds a large increased risk of visual impairment in people with schizophrenia compared to people without schizophrenia. There was a medium-sized effect of thinner overall peripapillary retinal nerve fibre layer thickness and small effects of thinner nasal and…
Peripheral vascular disease
How is peripheral vascular disease related to schizophrenia? People with schizophrenia show increased rates of co-occurring conditions. Peripheral vascular disease involves reduced circulation of blood to a body part other than the brain or heart, usually the legs, kidneys, or less commonly, the arms. The main cause of peripheral vascular disease is a build-up of fatty deposits that narrow blood vessels and reduce circulation of blood to the associated body part. What is the evidence for comorbid peripheral vascular disease? Moderate quality evidence finds no increases in peripheral vascular disease in people with schizophrenia compared to people without schizophrenia. June…

Polycistic ovary syndrome
We have not found any systematic reviews on this topic that meet the Schizophrenia Library’s inclusion criteria. Pending enough primary studies, we invite reviews on this topic to be conducted. Alternatively, we will endeavour to conduct our own review to fill this gap in the Library. June 2020

Postoperative complications
What are postoperative complications? The postoperative period starts from the time patients are transferred to the post-anaesthesia unit until they are released from hospital. Postoperative complications in people with schizophrenia may stem from disorganised thinking and functional difficulties that may affect the ability to recognise and communicate medical symptoms. Consequently, patients may be admitted for treatment at a later stage of the physical illness leading to increased risk of medical complications following surgery. What is the evidence for postoperative complications in people with schizophrenia? Moderate quality evidence suggests people with schizophrenia who have recently undergone surgery may show increased risk…

Reproductive and urological disorders
How are reproductive and urological dysfunction related to schizophrenia? People with schizophrenia may show increased rates of co-occurring conditions. These may include disorders of the reproductive organs or urological diseases. What is the evidence for comorbid reproductive and urological dysfunction? Moderate to low quality evidence suggests males (but not females) have increased risk of mortality due to urogenital disease compared to people without schizophrenia. There are also increased rates of obstetric complications in mothers with schizophrenia. June 2020

Respiratory system dysfunction
How are respiratory conditions related to schizophrenia? In general, people with schizophrenia are reported to have increased rates of co-occurring conditions. These may include disorders of the respiratory system, such as chronic obstructive pulmonary disease. What is the evidence for comorbid respiratory conditions? Moderate to high quality evidence suggests people with schizophrenia have increased rates of respiratory problems in general, low cardiorespiratory fitness, chronic obstructive pulmonary disease, and deteriorating lung capacity. They also have an increased risk of mortality due to respiratory illness compared to the general population. High rates of smoking may explain these associations. Exercise improves cardiorespiratory fitness,…
Sexual dysfunction
What is sexual dysfunction? Sexual dysfunction can take many forms, but affects both men and women, and can have far-reaching implications on self-esteem, quality of life, and relationships, as well as considerably reducing medication compliance should they cause sexual dysfunction. This table outlines the prevalence and causes of sexual dysfunction in people with schizophrenia. Please also see the relevant pharmaceutical treatment topic. What is the evidence for sexual dysfunction? Moderate to low quality evidence finds high levels of sexual dysfunction in both men and women with schizophrenia (between 25% and 85%). Factors associated with sexual dysfunction were increased symptom severity…

Skin disorders
What are skin disorders in schizophrenia? People with schizophrenia often show increased rates of co-occurring conditions, including skin disorders. Psoriasis is a long-term autoimmune condition that accelerates the life cycle of skin cells. This allows cells to build up on the surface of the skin, which form scales and red patches that are often itchy and painful. Pemphigoid is a rare autoimmune disorder that can develop at any age, but is most often seen in elderly patients. It results in skin rashes and blistering on the legs, arms, and abdomen. Alopecia areata is another autoimmune disease, but rather than affecting…

Sleep apnea
How is sleep apnea related to schizophrenia? People with schizophrenia may show increased rates of co-occurring conditions including sleep apnea. The most common form of sleep apnea is obstructive sleep apnea, which occurs when the muscles of the upper airway relax in such a way that they block the airway during sleep. As a result, obstructive sleep apnea is associated with daytime sleepiness, cognitive dysfunction, and the development of hypertension, cardiovascular disease, and abnormalities in glucose metabolism. Obstructive sleep apnea also has adverse effects on quality of life, and can lead to anxiety and depression symptoms. What is the evidence…

Thyroid disorders
How are thyroid disorders related to schizophrenia? People with schizophrenia may show increased rates of co-occurring conditions, including thyroid disorders. The thyroid gland makes hormones that help control many of the body’s metabolic processes, such as heart rate, blood pressure, body temperature and weight. If the thyroid becomes deregulated (overactive or underactive), or cancerous, this can result in a range of symptoms, including depression. What is the evidence for thyroid disorders in people with schizophrenia? Moderate to high quality evidence finds a small increase in the rate of Graves’ disease in people with schizophrenia or other psychotic disorders. June 2020

Underweight
How is being underweight relevant to schizophrenia? Being overweight is common in people with schizophrenia, usually due to lifestyle and side effects of medications, with adverse effects on health. However, being underweight also poses health risks such as ischemic heart disease. The causes of being underweight among patients are not fully understood, although genetics, metabolism, drug use, over-exercise, lack of food, and comorbid medical conditions can all affect weight status. What is the evidence for being underweight? Moderate quality evidence suggests the prevalence of being underweight is two times higher in people with schizophrenia than controls. Around 6% of people…
Venous thromboembolism
What is venous thromboembolism in schizophrenia? Venous thromboembolism is a disorder that includes deep vein thrombosis and pulmonary embolism. A deep vein thrombosis occurs when a blood clot forms in a deep vein, usually in the lower leg, thigh, or pelvis. Swelling, redness, and pain are some of the symptoms of deep vein thrombosis. A pulmonary embolism occurs when a clot breaks loose and travels through the bloodstream to the lungs. A pulmonary embolism can cause sudden chest pain and shortness of breath. What is the evidence for comorbid venous thromboembolism? Moderate to low quality evidence finds people with schizophrenia…
Green - Topic summary is available.
Orange - Topic summary is being compiled.
Red - Topic summary has no current systematic review available.
