Magnetic resonance imaging
What is magnetic resonance imaging (MRI)?
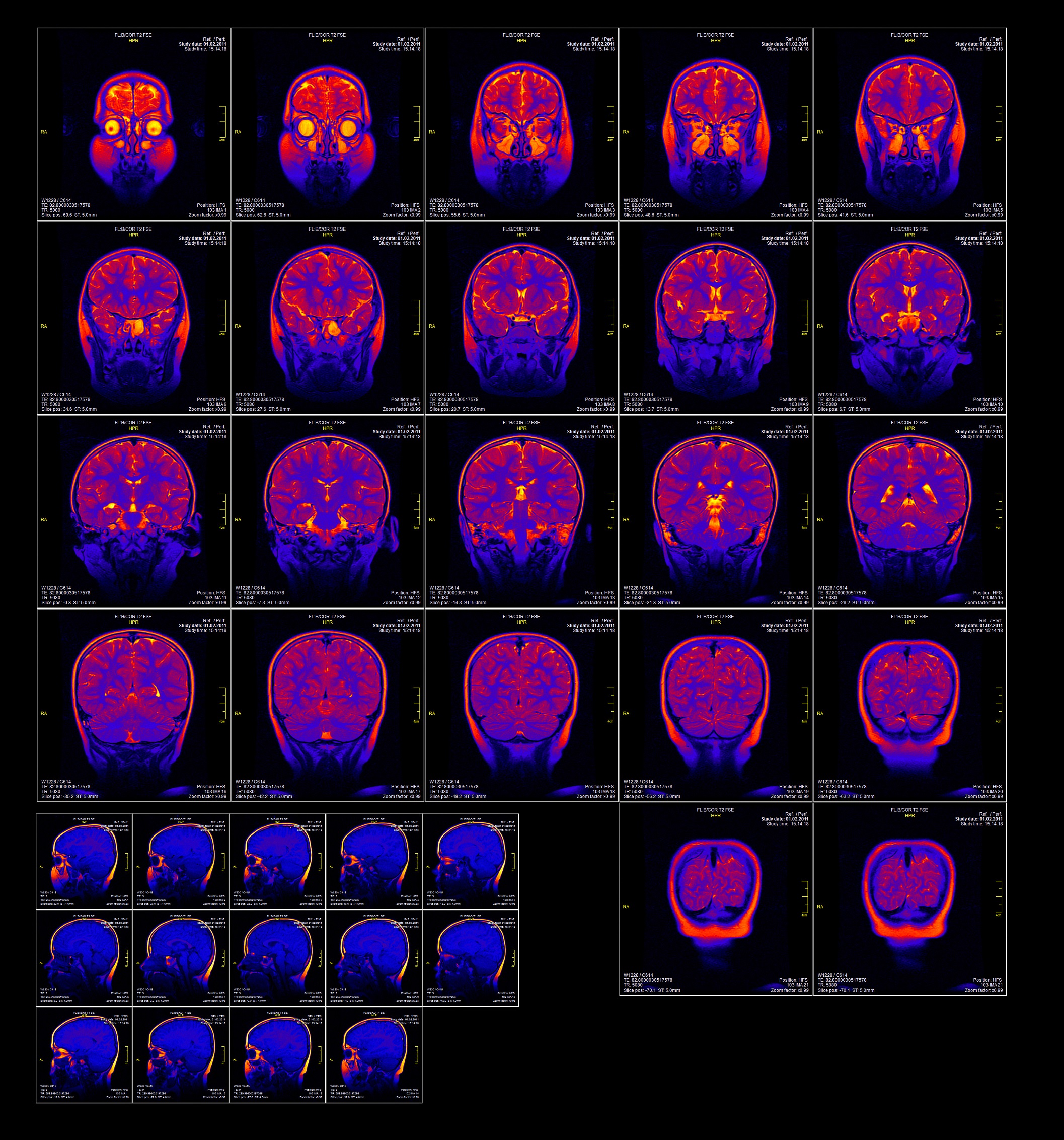
MRI is a used to visualise the structure of the brain and other regions of the body. It uses the magnetic properties inside cells (such as protons) to create a 3D image of the target region. Understanding structural brain alterations in people with schizophrenia may help understand changes in brain development associated with the illness onset or progression, and may help to inform future treatment strategies.
What is the evidence for MRI brain structure?
Moderate to high quality evidence found grey matter reductions in bilateral frontal lobe, anterior and posterior cingulate gyri, superior and medial temporal gyrus, inferior parietal gyrus, corpus callosum, cerebellum, thalamus (particularly mediodorsal, and an absent adhesio interthalamica), insula, amygdala, hippocampus, and parahippocampus in people with schizophrenia compared to controls. Volume increases were found in the caudate, putamen, right globus pallidus, cerebrospinal fluid, and ventricles (lateral, third, and fourth, and a large cavum septum pellucidum). There were white matter reductions in bilateral frontal lobe, anterior commissure, corpus callosum, fornix, internal capsule, left anterior segment of the arcuate fasciculus, left long segment of the arcuate fasciculus, bilateral arcuate fasciculus, bilateral cingulum, bilateral cortico-ponto-cerebellum tract, bilateral cortico spinal tract, bilateral inferior fronto-occipital fasciculus, bilateral inferior longitudinal fasciculus, bilateral inferior cerebellar penduculus, bilateral optic radiation, bilateral posterior segment of the arcuate fasciculus, bilateral superior longitudinal fasciculus 1, 2 and 3, bilateral superior cerebellar penduculus, and bilateral uncinate fasciculus. Moderate to low quality evidence found an absence of normal leftward asymmetry in the planum temporale and Sylvian fissure, and an excess rightward asymmetry in the superior temporal gyrus (particularly posterior). There was also a higher frequency of abnormal (reversed) asymmetry in the frontal and occipital lobes in people with schizophrenia than controls.
Moderate to high quality evidence found auditory hallucinations were associated with grey matter volume reductions in the left superior temporal gyrua, and lower quality evidence also found associations with reductions in insula grey matter volume. Patients with persistent negative symptoms showed reductions in bilateral medial frontal gyrus, left precentral gyrus, left middle frontal gyrus, left caudate nucleus (caudate head), bilateral parahippocampal gyri, left anterior cingulate, thalamus, and insula.
Moderate quality evidence found similar patterns of grey matter abnormalities in antipsychotic-naïve and treated first-episode patients (compared to controls) in the frontal (gyrus rectus), superior temporal, left hippocampal, and insula cortex. Grey matter in the left supramarginal gyrus and left middle temporal gyrus were increased in antipsychotic-naive patients, but decreased in treated patients, while left median cingulate/paracingulate gyri and right hippocampus grey matter were decreased in antipsychotic-naive patients, but increased in treated patients. There was also reduced grey matter volume in the cerebellar vermic lobule IV/V/VII, left cerebellar lobule IV/V, and left cerebellar Crus I in antipsychotic-naïve patients. Increased antipsychotic dose over time (>2 years) was associated with small decreases in parietal and occipital lobe volume, and small increases in basal ganglia volume.
Moderate quality evidence found regions of structural and functional overlap in drug-free patients compared to controls. There was decreased grey matter volume and decreased functional activity in the left medial posterior cingulate/paracingulate gyrus, right temporal pole/superior temporal gyrus, left fusiform gyrus, left inferior parietal gyrus, and left caudate nucleus. There was decreased grey matter volume and increased functional activity in the left superior temporal gyrus, right superior temporal gyrus, left fusiform gyrus, and right lingual gyrus. There was increased grey matter volume and decreased functional activity in the left cerebellum, right gyrus rectus, and right inferior parietal gyrus. There was increased grey matter volume and increased functional activity in the left insula and left cerebellum (lobule IX).
Compared to people with bipolar disorder, moderate to high quality evidence found small reductions in the amygdala, left insula, bilateral hippocampal regions in people with schizophrenia. There was a distinct region of the pregenual cingulate cortex (anterior Brodmann area 24) where grey matter reduction was detected in bipolar disorder and not schizophrenia. Compared to people with an autism spectrum disorder, moderate to low quality evidence found overlapping grey matter volume decreases in the right posterior cingulate cortex, right parahippocampus, and right putamen, and to a lesser extent the right insula and left thalamus.
Moderate quality evidence found people at high genetic risk for schizophrenia showed reduced hippocampus, anterior cingulate, left basal ganglia/claustrum, left thalamus/putamen, right superior frontal gyrus, left insula, left inferior temporal gyrus, and right inferior network, as well as increased left medial frontal gyrus and third ventricle volume compared to controls. People at high clinical risk for schizophrenia showed decreases in the parahippocampus, hippocampus, right anterior cingulate, insula, right middle/superior temporal gyrus, right inferior frontal gyrus, and right frontal gyrus compared to controls. People at high clinical risk showed decreases in the bilateral anterior cingulate compared to people at high genetic risk, and people at high genetic risk showed decreases in the left parahippocampus, insula, and right superior temporal gyrus compared to people at high clinical risk. Moderate to low quality evidence found high risk individuals who transitioned to psychosis had greater pituitary volumes compared to controls and reduced grey matter in the insula, cingulate cortex, superior temporal gyrus, prefrontal cortex, and cerebellum compared to high risk individuals who did not transition to psychosis.
October 2020
Fact Sheet Technical Commentary
Green - Topic summary is available.
Orange - Topic summary is being compiled.
Red - Topic summary has no current systematic review available.